NextGen 2024: Refractory SJIA & MAS Session Part 1
 AI Summary
AI Summary
Key Insights
- Outcomes for children with SJIA have improved with cytokine-directed biologic therapy, but some children still have a treatment refractory course.
- Refractory SJIA is broadly defined as a failure to respond to IL-1 and IL-6 blocking biologics, or having at least 2 episodes of MAS in 2 years, or development of SJIA-LD.
- A 'persistent partial MAS' is defined as a patient with active SJIA and persistent inflammation, with new or worsening lab results for at least 6 weeks.
- New refractory courses include IBD and lung disease, or 'SJIA-LD,' which encompasses several disease phenotypes.
- Atypical rashes in systemic JIA may not always be DRESS.
Loading...
Loading...
Loading...
Loading...
Loading...
Loading...
Loading...
Loading...
Loading...
Loading...
NextGen 2024: Refractory SJIA & MAS Session Part 1
- 1. The changing face of SJIA Grant Schulert, MD PhD Associate Professor of Pediatrics Division of Rheumatology, Cincinnati Children’s Hospital Medical Center Department of Pediatrics, University of Cincinnati College of Medicine
- 2. Complicated or refractory SJIA • Outcomes for children with SJIA have markedly improved with introduction of cytokine-directed biologic therapy (principally anti-IL-1 and IL-6) • However, some children fail to respond or have a treatment refractory course • Can include: – Persistent systemic features – Persistent arthritis – Steroid dependence – Recurrent macrophage activation syndrome including subclinical or “persistent partial MAS” – Other complications including lung disease
- 3. Defining refractory SJIA • Refractory SJIA (broadly) – Failure to respond to IL-1 AND IL-6 blocking biologics (failure=inability to resolve arthritis, systemic symptoms, or liver dysfunction, or being glucocorticoid dependent) OR – ≥2 episodes of MAS in a 2 year period OR – Development of SJIA-LD Canna et al (2020) PROJ 18(Suppl1):53
- 4. Defining refractory SJIA • “Persistent partial MAS” – A patient with active SJIA and persistent inflammation – Newly worsening or persistently abnormal laboratory features consistent with MAS for at least 6 weeks • Liver abnormalities • Disorders of hematopoiesis • Coagulopathy • Elevated IL-18 and CXCL9 – Does not meet criteria for overt MAS Canna et al (2020) PROJ 18(Suppl1):53
- 5. What is refractory SJIA biologically? • Most severe patients (correct treatments but strong not enough)? • Different disease phenotype (different pathways and needing different treatments)? • Unable to tolerate treatments (side effects or drug reactions)? • Complications triggered by treatments
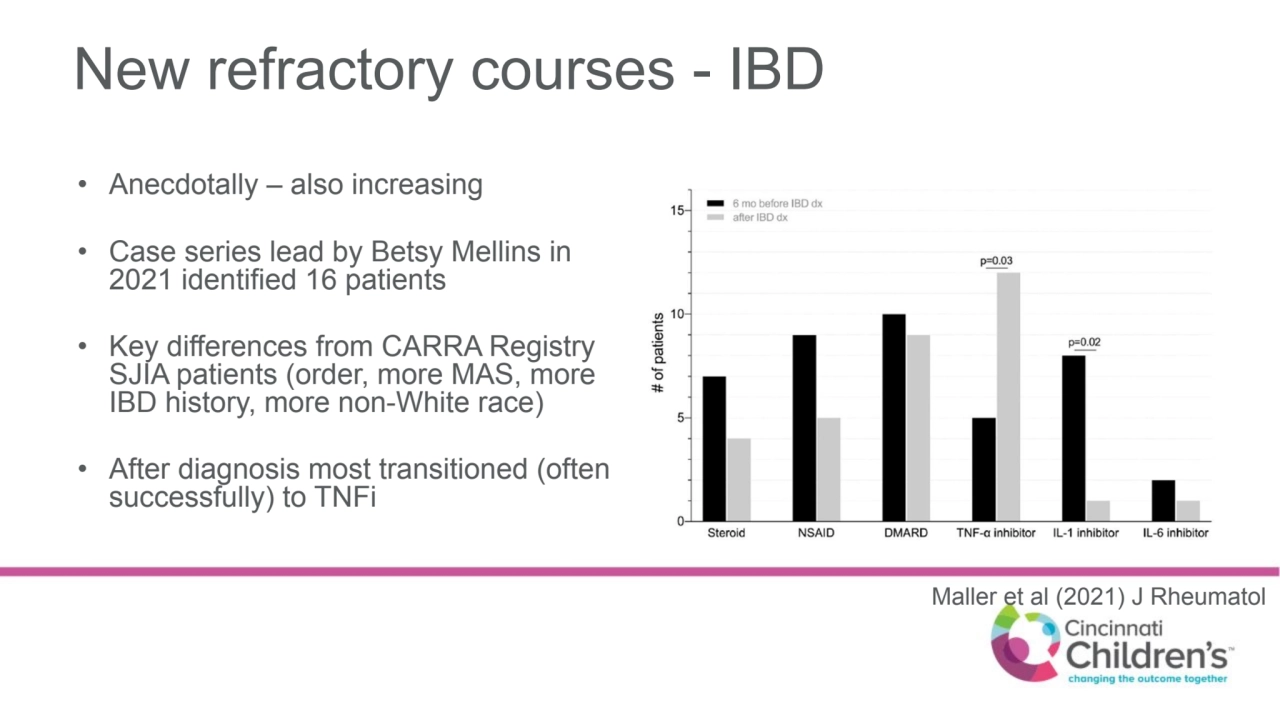
- 6. New refractory courses - IBD • Anecdotally – also increasing • Case series lead by Betsy Mellins in 2021 identified 16 patients • Key differences from CARRA Registry SJIA patients (order, more MAS, more IBD history, more non-White race) • After diagnosis most transitioned (often successfully) to TNFi Maller et al (2021) J Rheumatol
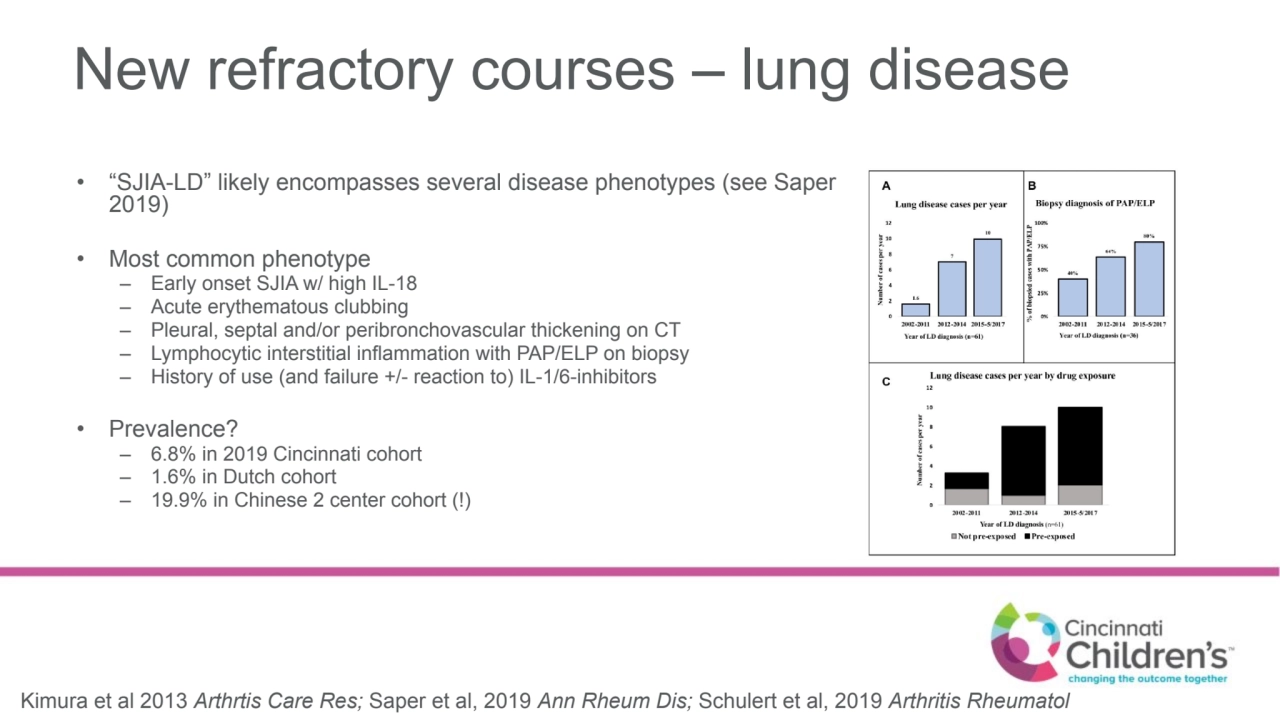
- 7. New refractory courses – lung disease • “SJIA-LD” likely encompasses several disease phenotypes (see Saper 2019) • Most common phenotype – Early onset SJIA w/ high IL-18 – Acute erythematous clubbing – Pleural, septal and/or peribronchovascular thickening on CT – Lymphocytic interstitial inflammation with PAP/ELP on biopsy – History of use (and failure +/- reaction to) IL-1/6-inhibitors • Prevalence? – 6.8% in 2019 Cincinnati cohort – 1.6% in Dutch cohort – 19.9% in Chinese 2 center cohort (!) Kimura et al 2013 Arthrtis Care Res; Saper et al, 2019 Ann Rheum Dis; Schulert et al, 2019 Arthritis Rheumatol
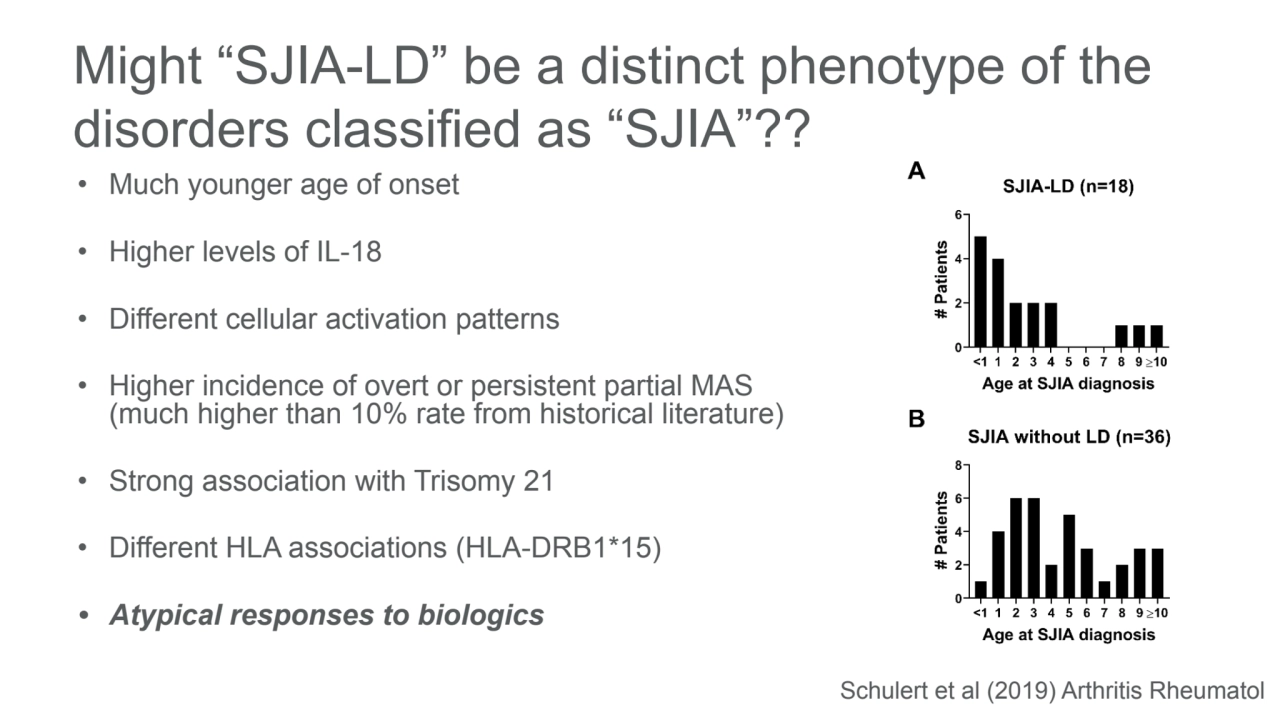
- 8. Might “SJIA-LD” be a distinct phenotype of the disorders classified as “SJIA”?? • Much younger age of onset • Higher levels of IL-18 • Different cellular activation patterns • Higher incidence of overt or persistent partial MAS (much higher than 10% rate from historical literature) • Strong association with Trisomy 21 • Different HLA associations (HLA-DRB1*15) • Atypical responses to biologics Schulert et al (2019) Arthritis Rheumatol
- 9. Atypical rashes in systemic JIA - definitely bad but maybe not always DRESS? • 30 patients with atypical rashes vs xx with “typical” Stills rash – Fixed urticaria, fixed macular and/or papular rash, pigmented or dyschromic (hyper- and/or hypochromic) papules or plaques, erythema and/or edema of the eyelids and back of the hands (dermatomyositis-like), scaly-crusted erythema. • Atypical rashes had higher CRP and ferritin at onset, more MAS (27% vs 10%), more failure of first-line Rx, more biologics needed, and more likely to have persistent disease course (biologics 2+ years from diagnosis) J Am Acad Dermatol (2022) 87:1445
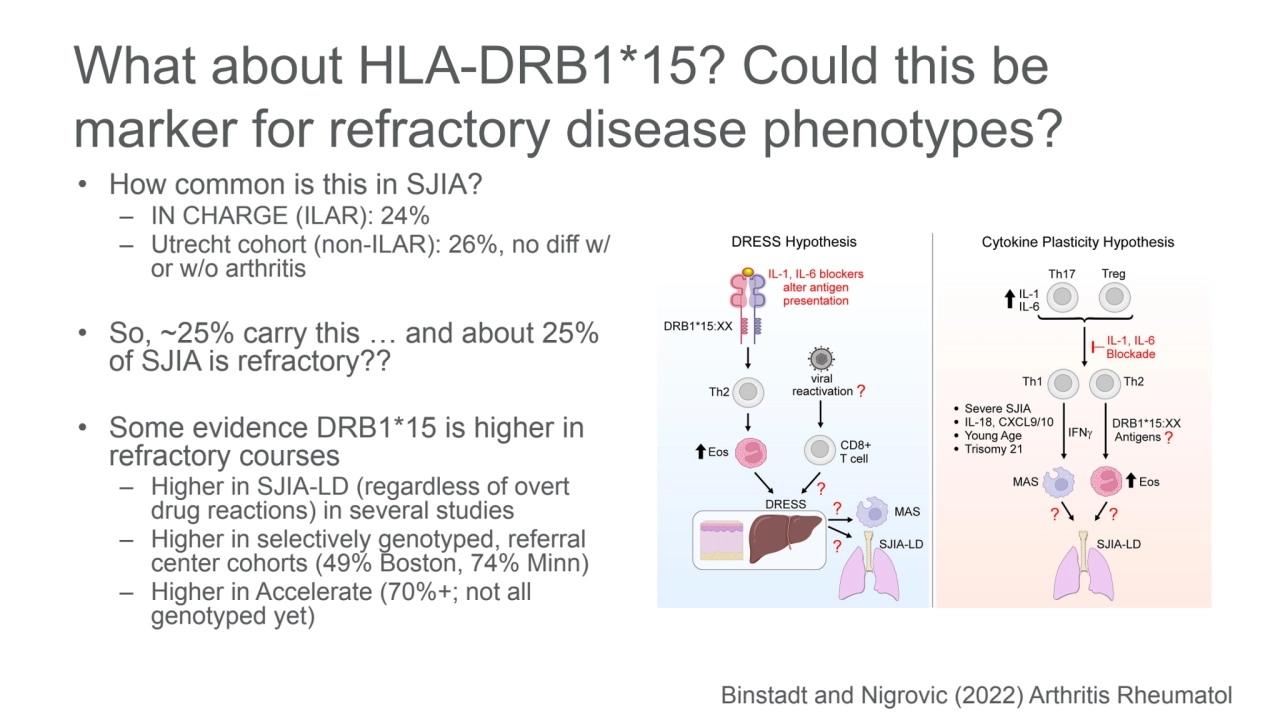
- 10. What about HLA-DRB1*15? Could this be marker for refractory disease phenotypes? • How common is this in SJIA? – IN CHARGE (ILAR): 24% – Utrecht cohort (non-ILAR): 26%, no diff w/ or w/o arthritis • So, ~25% carry this … and about 25% of SJIA is refractory?? • Some evidence DRB1*15 is higher in refractory courses – Higher in SJIA-LD (regardless of overt drug reactions) in several studies – Higher in selectively genotyped, referral center cohorts (49% Boston, 74% Minn) – Higher in Accelerate (70%+; not all genotyped yet) Binstadt and Nigrovic (2022) Arthritis Rheumatol